Keratoconus
Keratoconus
Comprehensive Guide to Causes, Symptoms, Diagnosis, and Treatment Options

Introduction to Keratoconus
Keratoconus is a progressive eye condition where the normally round cornea thins and gradually bulges outward into a cone-like shape. This distortion prevents light from focusing properly on the retina, leading to blurred, distorted, or irregular vision. It typically affects both eyes, though one may be more severe, and often begins in the teenage years or early adulthood, progressing over 10–20 years before stabilizing.
Recent global studies estimate keratoconus affects approximately 289 per 100,000 people (about 1 in 345), with prevalence rising due to improved diagnostics—over 23 million individuals worldwide are impacted. It’s more common in certain regions (e.g., higher in Africa and parts of Asia) and among males, with peak incidence in the 20–29 age group.
At The Scleral Lens Center in Central Ohio, under the leadership of Dr. Greg DeNaeyer, we specialize in advanced management of keratoconus using custom scleral lenses. Dr. DeNaeyer, with over 25 years of expertise in specialty contact lenses, has lectured worldwide and contributed to research on corneo-scleral topography and scleral lens fitting—key tools for optimizing outcomes in irregular corneas like those in keratoconus.
Keratoconus isn’t just a vision issue; it can significantly affect daily life, from driving to reading or screen work. Early intervention is essential to preserve vision and quality of life.

Causes and Risk Factors of Keratoconus
The exact cause remains unclear, but it’s believed to involve a combination of genetic, environmental, and biochemical factors:
- Genetic Predisposition: Family history increases risk; certain genes linked to collagen structure play a role.
- Environmental Triggers: Chronic eye rubbing (often from allergies)
- Biochemical Changes: Reduced corneal collagen cross-links lead to weakening and ectasia (bulging).
- Associated Conditions: Allergies, atopy, connective tissue disorders (e.g., Ehlers-Danlos), or Down syndrome elevate risk.
Eye rubbing is a strong modifiable factor—patients with keratoconus often report vigorous rubbing, which can accelerate progression.

Common Symptoms of Keratoconus
Symptoms typically start subtly and worsen over time:
- Blurred or Distorted Vision: Straight lines appear wavy; double or ghost images common.
- Increased Astigmatism: Rapid prescription changes; glasses often inadequate.
- Light Sensitivity and Glare: Halos, starbursts, or difficulty with night vision.
- Frequent Headaches or Eye Strain: From squinting or poor focus.
- Difficulty Driving at Night: Due to glare and reduced contrast.
Early stages may mimic myopia or astigmatism, delaying diagnosis.
Diagnosing Keratoconus
Diagnosis requires specialized testing beyond a standard eye exam:
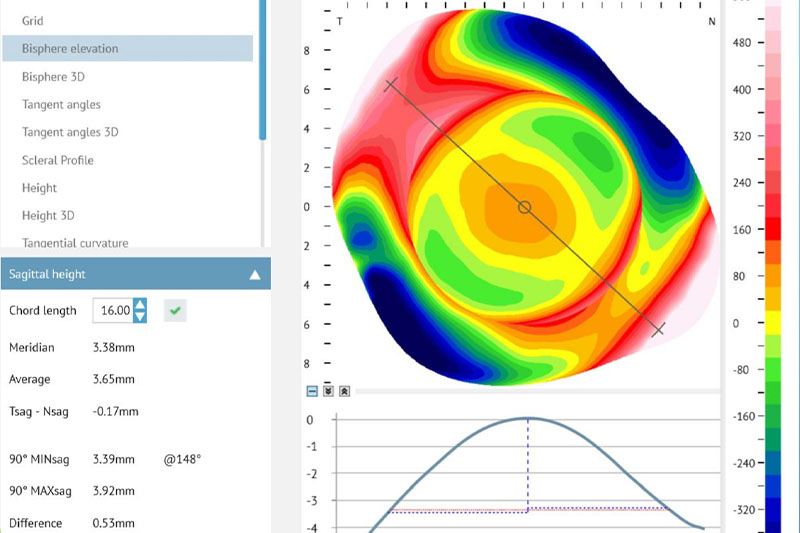
- Corneal Topography/Tomography: Gold standard (e.g., Pentacam) maps shape, detecting cone-like steepening and thinning.
- Pachymetry: Measures corneal thickness (often <500 μm in affected areas).
- Aberrometry: Quantifies higher-order aberrations causing distortion.
- Slit-Lamp Biomicroscopy: Reveals signs like Fleischer’s ring, Vogt’s striae, or apical scarring.
- Refraction and Visual Acuity: Assesses best-corrected vision.
At The Scleral Lens Center, Dr. DeNaeyer employs advanced tomography and profilometry—areas of his published expertise—to accurately stage keratoconus and guide lens design.
Treatment and Management Strategies for Keratoconus
There’s no cure, but treatments halt progression and restore vision:
Early-Stage Options
- Glasses or Soft Contacts: Sufficient initially but often fail as irregularity increases.
- Corneal Cross-Linking (CXL): Strengthens collagen bonds with UV light and riboflavin; halts progression in 90%+ of cases when done early.
Vision Correction: Scleral Lenses – The Preferred Choice for Many

Scleral lenses are large-diameter, gas-permeable lenses that vault over the cornea and rest on the sclera, filled with saline to create a smooth optical surface.
Key Benefits for Keratoconus:
- Superior Vision Correction: Neutralizes irregular astigmatism; many achieve 20/30 or better (studies show 80–90% success in significant improvement).
- Enhanced Comfort: No corneal contact reduces irritation and abrasions.
- Stability and All-Day Wear: Less movement; ideal for active patients.
- Corneal Protection: Shields from rubbing/environmental factors.
- High Success Rate: Clinical data indicate 85–95% of properly fitted patients experience marked improvement in vision and quality of life; long-term studies affirm safety and efficacy.
Dr. Greg DeNaeyer excels in fitting scleral lenses for keratoconus, drawing from his research on scleral shape/topography. Custom designs (e.g., free-form or multi-meridian) ensure optimal vault, minimal fogging, and maximal clarity—even in advanced cases.
Other Advanced Options
- Rigid Gas-Permeable (RGP) or Hybrid Lenses: Alternatives but less comfortable than sclerals.
- Intacs: Intracorneal rings to flatten the cone in select cases.
- Corneal Transplant: Last resort for severe scarring or hydrops (rare with modern management).
Scleral lenses often delay or avoid transplant—studies show rigid/scleral lens users have up to 80% lower transplant risk.
Living with Keratoconus
- Avoid eye rubbing.
- Use allergy management to reduce triggers.
- Schedule regular monitoring (every 6–12 months).
- Maintain eye hygiene for lens wear.
Support groups and resources help with emotional impact.
Frequently Asked Questions About Keratoconus
Is keratoconus hereditary?
Partially—genetic factors increase risk, but environmental triggers play a role.
Can scleral lenses stop progression?
They don’t halt progression like CXL, but provide excellent vision and may reduce rubbing-related worsening.
How long do scleral lenses last?
With care, 1–3 years; regular check-ups ensure fit and eye health.
Are scleral lenses suitable for all keratoconus stages?
Yes—from mild to advanced; often the best non-surgical option.
What triggers progression?
Eye rubbing
Conclusion: Effective Management Starts Here

Keratoconus is manageable—with early CXL to stabilize and scleral lenses to restore clear, comfortable vision. At The Scleral Lens Center, Dr. Greg DeNaeyer’s expertise in specialty lenses for irregular corneas ensures personalized, high-success fittings that transform vision.
If you suspect keratoconus or have been diagnosed, contact us for a comprehensive evaluation. Regain sharp, stable sight—schedule your consultation today.