Sjogren’s Syndrome

Introduction to Sjogren’s Syndrome
Sjogren’s syndrome, pronounced “SHOW-grins,” is a chronic autoimmune disorder where the body’s immune system mistakenly attacks its own moisture-producing glands, leading to persistent dryness, particularly in the eyes and mouth. Named after Swedish ophthalmologist Henrik Sjogren, this condition affects an estimated 3-4 million people in the United States, with women comprising about 90% of cases, often diagnosed between ages 40 and 60. It can occur alone (primary Sjogren’s) or alongside other autoimmune diseases like rheumatoid arthritis or lupus (secondary Sjogren’s).
Dry eye is one of the hallmark symptoms, resulting from inflammation of the lacrimal glands, which reduces tear production and leads to ocular surface damage if untreated. Beyond dryness, Sjogren’s can cause systemic issues, including fatigue, joint pain, and increased risk of lymphoma. At The Scleral Lens Center, under the expert leadership of, we focus on ocular manifestations, offering specialized treatments like scleral lenses to alleviate severe dry eye associated with this disease. Dr. DeNaeyer is internationally recognized for his work in specialty contact lenses, having delivered lectures and workshops at over 70 conferences worldwide and authored over 50 professional publications, including key articles on scleral lenses for dry eye conditions like “Scleral Lenses: An Overlooked Fix for Dry Eye?” and research on scleral shape in the SSSG Study. As a co-founder and past president of the Scleral Lens Education Society, and a Fellow of the American Academy of Optometry, he brings unparalleled expertise to our patients, having traveled globally to advance eye care practices. This guide provides a thorough exploration of Sjogren’s, empowering you with knowledge for better management.
Causes and Risk Factors of Sjogren’s Syndrome
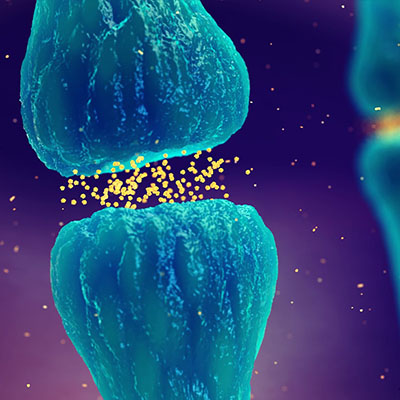
The exact cause of Sjogren’s remains unclear, but it’s believed to involve a combination of genetic predisposition and environmental triggers. The immune system produces autoantibodies that target exocrine glands (those secreting fluids like tears and saliva), causing lymphocytic infiltration and gland dysfunction.

Genetic and Immune Factors
Family history increases risk, with certain genes linked to immune regulation playing a role. Viral infections (e.g., Epstein-Barr) may trigger the autoimmune response in susceptible individuals.
Hormonal Influences
Estrogen fluctuations explain the higher incidence in women, particularly post-menopause, when hormonal changes exacerbate gland inflammation.

Environmental Triggers
Exposure to certain viruses, bacteria, or chemicals might initiate the disease. Smoking and stress can worsen symptoms.
Risk factors include age (over 40), female gender, and co-existing autoimmune conditions. Early detection is key, as dry eye often precedes other symptoms by years, and specialists like Dr. DeNaeyer emphasize proactive screening.
Common Symptoms of Sjogren’s Syndrome
Symptoms vary widely but center on sicca (dryness) complex.
Ocular Symptoms
- Severe Dry Eye: Gritty, burning sensation; redness; light sensitivity; blurred vision.
- Infections and Ulcers: Reduced tears increase risk of corneal issues.
- Itchiness and Fatigue: Eyes tire easily, worsening with screen use.
Dry eye affects up to 90% of patients, often the first sign.
Oral and Systemic Symptoms
- Dry Mouth (Xerostomia): Difficulty swallowing, speaking, or tasting; increased cavities and oral infections.
- Fatigue and Joint Pain: Chronic tiredness and arthritis-like aches.
- Other Manifestations: Dry skin, nose, or vagina; swollen salivary glands; nerve damage; lung, kidney, or neurological issues.
In advanced cases, complications like lymphoma (5-10% risk) or vision loss from corneal scarring may occur.
Diagnosing Sjogren’s Syndrome
Diagnosis can take years due to subtle onset. It follows criteria from the American College of Rheumatology/European League Against Rheumatism (ACR/EULAR), requiring at least 4 points from tests like positive anti-SSA antibodies, low tear/saliva flow, or gland biopsy showing inflammation.
Key Diagnostic Tests

- Blood Tests: Detect autoantibodies (anti-SSA/Ro, anti-SSB/La), rheumatoid factor, and elevated inflammation markers.
- Schirmer’s Test and Ocular Staining: Measure tear production and surface damage.
- Salivary Gland Biopsy: Confirms lymphocytic infiltration.
- Sialometry: Assesses saliva flow.
- Imaging: Ultrasound or MRI of glands.
Eye care providers often play a pivotal role, as dry eye prompts initial evaluation. Multidisciplinary care involving rheumatologists is recommended, and at our center.
Treatment and Management of Sjogren’s Syndrome
There’s no cure, but treatments focus on symptom relief, inflammation control, and complication prevention.
Systemic Treatments
Immunosuppressants like hydroxychloroquine or methotrexate manage joint pain and fatigue. Biologics (e.g., rituximab) target B-cells in severe cases. Pilocarpine or cevimeline stimulate saliva/tear production.
Ocular-Specific Therapies
For dry eye:
- Artificial Tears and Gels: Preservative-free for frequent use.
- Anti-Inflammatory Drops: Cyclosporine or steroids reduce gland inflammation.
- Punctal Plugs: Conserve tears.
- IPL or LipiFlow: Address associated MGD.
Scleral Lenses: Optimal Relief for Sjogren’s-Related Dry Eye

Scleral lenses are a game-changer for Sjogren’s patients with severe dry eye. These vaulted lenses create a saline-filled chamber over the cornea, providing continuous hydration and protection from evaporation and lid friction. They also correct vision distortions caused by irregular surfaces.
Scleral Lenses provide:
- Hydration and Comfort: Bathes the eye all day, alleviating burning and grittiness.
- Barrier Protection: Shields from irritants, reducing infections.
- Vision Enhancement: Smooths the ocular surface for clearer sight.
- Suitability for Autoimmune Eyes: Unlike soft lenses, they tolerate compromised surfaces well.
Studies confirm scleral lenses improve quality of life in Sjogren’s, often succeeding where drops fail. At The Scleral Lens Center, we use 3D mapping for precise fits, minimizing issues like fogging through optimized designs.
Lifestyle and Supportive Measures
Stay hydrated, use humidifiers, avoid irritants, and practice oral hygiene. Support groups and counseling help with emotional impacts.
Living with Sjogren’s Syndrome
Daily management includes monitoring for complications, regular check-ups, and adapting routines—e.g., carrying eye drops. Exercise and anti-inflammatory diets can mitigate fatigue.
Frequently Asked Questions About Sjogren’s Syndrome
Is Sjogren’s hereditary?
It has a genetic component but isn’t directly inherited; environmental factors trigger it.
Can Sjogren’s affect organs beyond eyes and mouth?
Yes, it can involve lungs, kidneys, nerves, and increase lymphoma risk.
Are scleral lenses suitable for all Sjogren’s patients?
Most with severe dry eye benefit, but fitting requires professional assessment.
How does Sjogren’s differ from regular dry eye?
It’s autoimmune-driven, often more severe and systemic.
What triggers Sjogren’s flares?
Stress, infections, or hormonal changes.
Conclusion: Empowering Your Journey with Sjogren’s
Sjogren’s syndrome demands vigilant management, but with treatments like scleral lenses, many lead fulfilling lives. At The Scleral Lens Center, led by Dr. Greg DeNaeyer—whose international travels, lectures, and publications have shaped modern scleral lens practices—we’re here to support your ocular health. Contact us for personalized care.
